The role of Occupational Therapy in Hand Trauma
by Helen Green
If we take a minute to think about what we have already done with our hands since waking up this morning, it is not only surprising, it is completely amazing. Not only do we use our hands physically for the majority of functional tasks we use them to communicate, gesture and for touch and human interaction. However, our hands are vulnerable and until something happens we inevitably take them for granted.
Hand Trauma
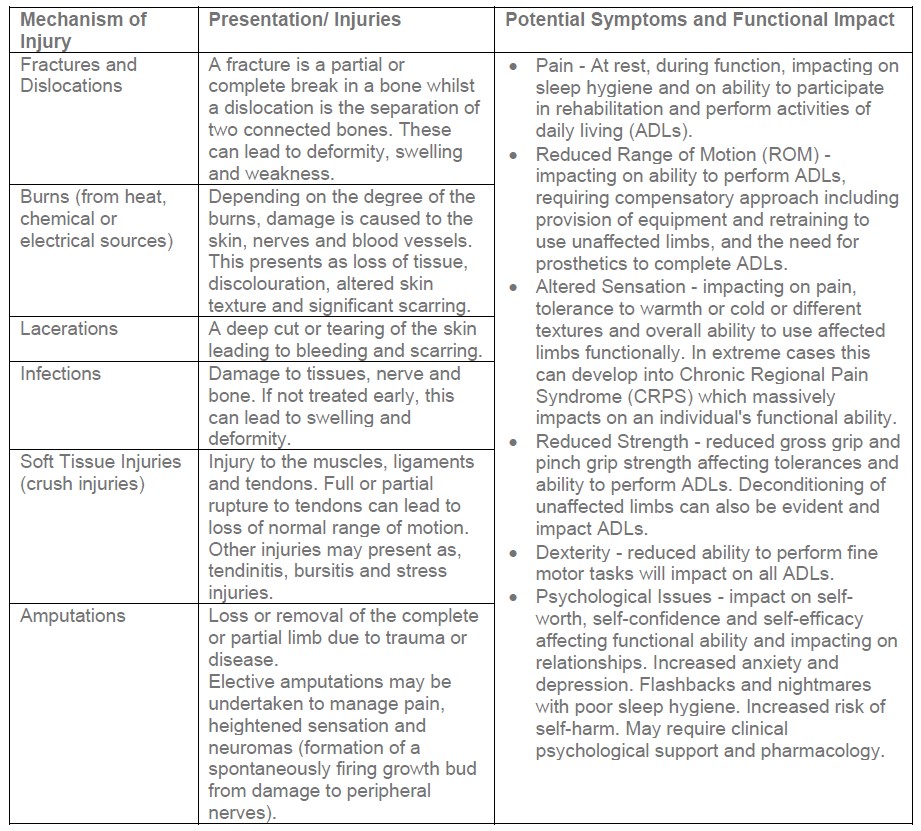
Hand trauma can occur over time or in a split second and subsequent injuries can be life changing. Hand trauma refers to any injury involving the fingers, hands and wrists. The table below demonstrates the different categories of hand trauma, their presentation, symptoms and the potential impact on function.
Role of the OT in the Acute Phase (0-3 months)
As part of the wider multi-disciplinary team (MDT), the OT has an important part to play in the immediate treatment of hand trauma. Most traumatic injuries involve multiple structures and systems and will require surgery. It is essential that the OT has a good understanding of anatomy, wound management, healing of tendons, ligaments and bones and how these impact on biomechanics and functional movement. In many hospitals, OTs are increasingly active as part of the theatre team, splinting during, before or immediately after surgery. This may be to reduce unstable fractures, immobilised tissues and prevent deformity and contracture of soft tissues.
Even at this early stage, the overall long-term aim is maximising function. The OT will also be involved in:
- Patient education
- Wound management
- Controlling oedema
- Pain management
- Psychological support
- Managing and protecting repairs to bones, tendons etc.
- Preventing joint stiffness in all uninvolved joints
- Scar management
- Initiating appropriately paced exercises with passive and active movements/exercises
- Setting goals
Pathways for Different Injuries
Orthopaedic hand surgeons and the MDT will follow a wide range of pathways and specific protocols for all types of traumatic injury and these can vary between different hospitals. Protocols and procedures can be requested to guide prognosis and rehabilitation. For example with flexor tendon injuries, the nerve may be severed and require surgical repair and splinting with a clear guidance on timescales and treatment. The nerve injury may cause loss of sensation affecting function and safety. The patient will need to be taught to take care with heat and sharp objects and to re-educate the brain through desensitisation techniques to recognise signals from peripheral nerves. Heightened sensitivity and intolerance to cold can last for up to two years post nerve injury.
Role of the OT in the Rehabilitation Process
Assessing and treating traumatic hand injuries can initially be quite daunting, however also hugely rewarding. First and foremost therapy needs to be tailored to the individual and the therapist must always demonstrate positivity and respect, recognising that the therapist’s priorities may well be different to the client’s priorities.
Therapists must provide realistic hope, build rapport, be good listeners and be trusted by the client. It is essential that the therapist appreciates the impact of the injuries on a client's mental health and ensures this is a key aspect of the rehabilitation process. The main goal of therapy is not necessarily regaining a "normal" hand, but maximising function with minimal pain.
Hand therapy assessment comprises of subjective and objective aspects and includes:
- Gaining consent.
- Establishing rapport.
- Getting a medical history - including understanding of co--morbidities which may impact rehabilitation and recovery.
- Getting a history of the current condition and mechanism of injury and how this was treated in the acute phase. Having prior sight of the Immediate Needs Assessment report and other relevant medical reports is extremely helpful for therapists, and also reduces the need for the patient to have to repeat and relive upsetting experiences.
- The impact of pain and ongoing management.
- Examination of hand limb posture, including any signs of neglect.
- Examination of skin, including healing of any grafts, flaps or other surgical wounds, texture, sweating, hair growth and scars. The status of the scars would be described including any hypersensitivity, as well as current and future scar management.
- Examination of soft tissues, including oedema, tendon integrity, muscle testing, gross (power) grip, and pinch grip.
- Examination of bones and joints, including bone alignment, joint integrity, ROM and stiffness.
- Assessing any sensory damage or injury to nerves, the need for further testing (nerve conduction studies), and any sensory pain and hypersensitivity. The overall impact of altered sensation on function and sleep and the need for desensitisation as part of treatment.
- Assessing dexterity and functional use of the hand, including patients’ own perceptions whilst considering their environment and relevant ADLs, hobbies and work requirements.
- Identifying the need for signposting or onward referral for other services such as clinical psychological assessment, orthopaedic review and employing a rehab assistant.
- Identifying the need for equipment or adaptations.
The Hand Therapy Rehabilitation Programme
Hand therapy treatment sessions will be dependent on the outcome of the evaluation, the client's wishes, funding approval and the goals set by both the therapist and the client. Treatment will always be clinically reasoned and include all or a combination of the following:
- Advice and education
- Scar/ wound management
- Desensitisation
- Splinting
- Increasing ROM
- Increasing power and pinch grip strength
- Increasing functional independence with ADLs, work and hobbies, including safe use of equipment
- Psychological support
It is important to note that depending on the skills of the treating hand therapist, they may also be able to address:
- Fatigue management
- Sleep hygiene
- Anxiety management
- Advice on adaptations to the home, workplace or vehicles
- Ergonomic assessments
- Vocational Rehabilitation
OTs will use a wide range of subjective and objective outcome measures and tools to provide baseline information and demonstrate subsequent improvement and progression of the treatment plan as well as evidence if plateauing of goals is occurring.
Other Considerations
There is inevitably and understandably a clear difference between the scope and duration of services that can be provided by the public versus the independent sectors.
Hand therapy is an essential component in the rehabilitation journey of a client following hand trauma and we work with many case managers throughout the UK who regularly refer their clients to us for this support. Hand therapists are both highly skilled and highly sought after in equal measure, this has led us to needing to find innovative ways to ensure we can meet the needs of clients with the hand therapy resource available. Thankfully, clients with hand injuries do not always have cognitive impairment and are therefore able to be proactive in their rehabilitation with ongoing education, advice and support from the therapist.
Assessment and treatment sessions will often be completed both face-to-face and remotely by video call which can prove more time efficient and cost-effective. I have even completed remote assessments and used a modified sphygmomanometer (adapted blood pressure cuff) set up and sent in advance to the patient to acquire strength measurements.
Often patients with finger and/or thumb amputations or significant crush injuries are particularly hindered functionally by severe sensory pain. This can lead to the development of neuromas and require consideration for further surgery and trauma, with outcomes that are not always successful. In these cases, it is worth considering referral for a Regenerative Peripheral Nerve Interface (RPNI) procedure, where the divided end of the peripheral nerve is implanted and embedded into a muscle graft. Links for further information on this are listed below. This novel technique is increasingly achieving reduced pain and sensation for patients who were previously unable to function due to the chronic sensory pain and also reduces the risk of neuromas re-occurring.
Conclusion
Specialist occupational therapists with their background training in physical and mental health are ideally placed to treat complex hand trauma. They treat the whole person not just the injured limb and fully understand the impact of upper limb dysfunction on every aspect of their patient's life. Outcomes will always be influenced by the patient's motivation and compliance, however the therapist will be patient, passionate and persevere to ultimately achieve maximum function.
When working with clients with hand trauma, a case manager should always consider referral to a specialist hand therapist as an essential part of their client’s rehabilitation and recovery. If you have a client who would benefit from a hand therapy assessment please contact the team on 0330 0249910 or enquiries@theotpractice.com.
Useful Links:

